Carol Randolph is severely allergic to bee stings and corn products, so for the past 20 years, the 55-year-old has to watch everything she consumes and what comes in contact with her body.
Common things such as hand sanitizers and powdered medical gloves can constrict her airways, cause her to break out in hives and turn her lips purple. An EpiPen, which was almost free at one time, can save her life. Now, even with her retired military insurance, it costs $100 every time she buys one.
“There wasn’t even a co-pay for an EpiPen,” Randolph of Munford, Tennessee, said. “Now I have to come up with $100 dollars to save my life.”
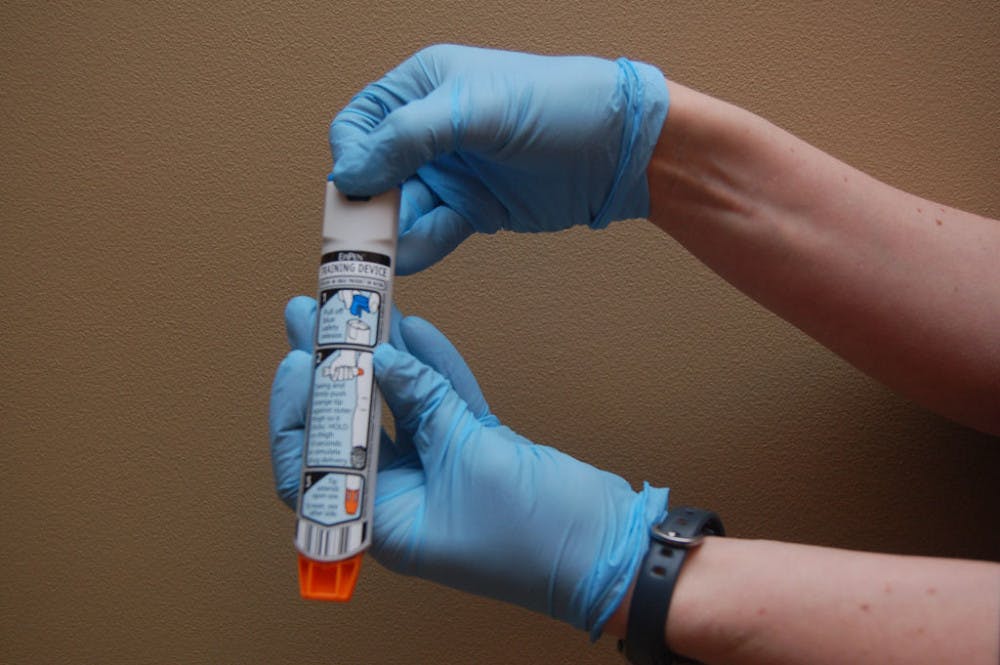
An EpiPen is an auto-injecting device that sends a drug called epinephrine into the blood stream when someone is having an allergic reaction. This shot of adrenaline causes the heart to beat faster and the airways to open up.
Millions of people with life-threatening allergies use EpiPens. In the past few years, the increasing price of an EpiPen has caused many people to question the healthcare system and their safety. For people such as Randolph, who need to keep an EpiPen within arm’s reach in case of an allergic reaction, paying more than $600 is almost unacceptable.
“This could financially wipe out a family or a senior citizen living on a fixed income,” Randolph said.
A pack of two EpiPens sold for $106.32 in Nov. 2004 as reported by the Elsevier Clinical Solutions’ Gold Standard Drug Database. As of May 2016, a two pack cost more than $600. Just three years ago, the price was only $252, meaning the price has doubled since 2013.
Mylan, the company who owns the patent for the EpiPen, has received criticism for raising the price of EpiPens. After buying the EpiPen in 2007, Mylan has increased revenue and awareness of the device. Alternate uses for epinephrine releases, such as Sanofi’s Auvi-Q, cannot quite match the brand recognition that Mylan has set with the EpiPen.
For EpiPen users who face higher out-of-pocket costs, Mylan is offering a savings card for up to $300. The company also is doubling eligibility for patient assistance program to 400 percent of the federal poverty level. A family of four making up to $97,200 would not pay out of pocket for their EpiPen. Mylan would continue focusing on offering EpiPens in schools, called the EpiPen4Schools program.
“The program, launched in August 2012, has provided more than 700,000 free epinephrine auto-injectors and educational resources to more than 65,000 schools nationwide to help them be prepared for anaphylaxis events among students,” the company said in a press release on Aug. 25.
Mylan CEO Heather Bresch told the House Oversight and Government Reform Committee members the company only makes $100 for every pack of EpiPens listed at $609 after rebates and other costs. Lawmakers accused Mylan of profiting from an inexpensive life-saving drug. The Federal Drug Administration has also faced backlash for not approving other company’s epinephrine injectors quickly enough. The FDA said they approved four products, but nothing has happened yet.
The general cost to patients for an EpiPen before insurance coverage is about $700, Amanda May, a clinical pharmacist at LeBonheur Children’s Hospital, said.
EpiPens are used for life-threatening allergic reactions in which anaphylaxis, a reaction in which the airway swells and a person stops breathing, occurs, May said. This can cause brain damage or death if not responded to immediately.
EpiPens currently last for 18 months from the manufacturing date. They are not reusable, so they need to be replaced after use or every 18 months.
Gina Swords, a mother from Millington, has a son who has been allergic to peanuts and amoxicillin since he was born.
“Last year, before the price went up, I had a free co-pay card,” Swords said. “I could get them refilled for nothing. So I stocked up on EpiPens.”
Swords said she had previously bought a two-pack from Walgreens for $50, but they expired in three months.
“Once they made EpiPens that didn’t have expiration dates, it was easy to get a lot and keep them,” Swords said. “You just have to watch the color of the medicine to know if it’s still good.”
Swords said she will not pay $600 for an EpiPen.
“We have been fortunate to not have to use an EpiPen in an emergency, but I still want to have them just in case,” Swords said.
EpiPens send epinephrine into the bloodstream of someone suffering from an allergic reaction. The devices were almost free at one point, but now cost $100.